February 4, 2020
Dual Loading of Nanoparticles with Doxorubicin and Icotinib for the Synergistic Suppression of Non-Small Cell Lung Cancer
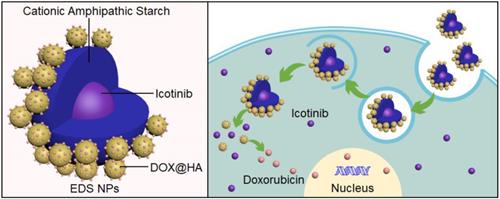
Background: Combination chemotherapy plays an important role in the clinical therapy of non-small cell lung cancer (NSCLC). However, the pharmacokinetic differences between drugs are an insurmountable barrier in traditional treatment. For the synergistic therapy of NSCLC, synergistic nanoparticles (EDS NPs) loaded with both an EGFR inhibitor and doxorubicin (DOX) were designed and prepared.
Methods: Erlotinib, apatinib and icotinib were evaluated for optimal combination with DOX in treatment of NSCLC via CCK-8 assay. Then the cationic amphipathic starch (CSaSt) and hyaluronic acid (HA) were applied to coencapsulate DOX and EGFR inhibitor to form the EDS NPs. EDS NPs were evaluated in NSCLC cell lines (A549, NCI-H1975 and PC9) and NSCLC xenograft mouse models.
Results: Icotinib was found to be the optimal synergistic drug in combination with DOX in the tested. Subsequently, icotinib and DOX were coencapsulated in the NPs. EDS NPs were roughly spherical with an average size of 65.7±6.2 nm and possessed stable loading and releasing properties. In the in vitro investigation, EDS NPs could efficiently deliver payloads into cells, exhibited cytotoxicity and produced strong anti-migration properties. In vivo hypotoxicity was confirmed by acute toxicity and hemolytic assays. The in vivo distribution showed that EDS NPs could enhance accumulation in tumors and decrease nonspecific accumulation in normal organs. EDS NPs significantly promoted the in vivo synergistic effects of icotinib and DOX in the mouse model.
Conclusions: The study suggests that EDS NPs possess noteworthy potential for development as therapeutics for NSCLC clinical chemotherapy.
Keywords: non-small cell lung cancer, combination chemotherapy, nanoparticles, icotinib, doxorubicin